- DATE:
- AUTHOR:
- Nicole Shelby
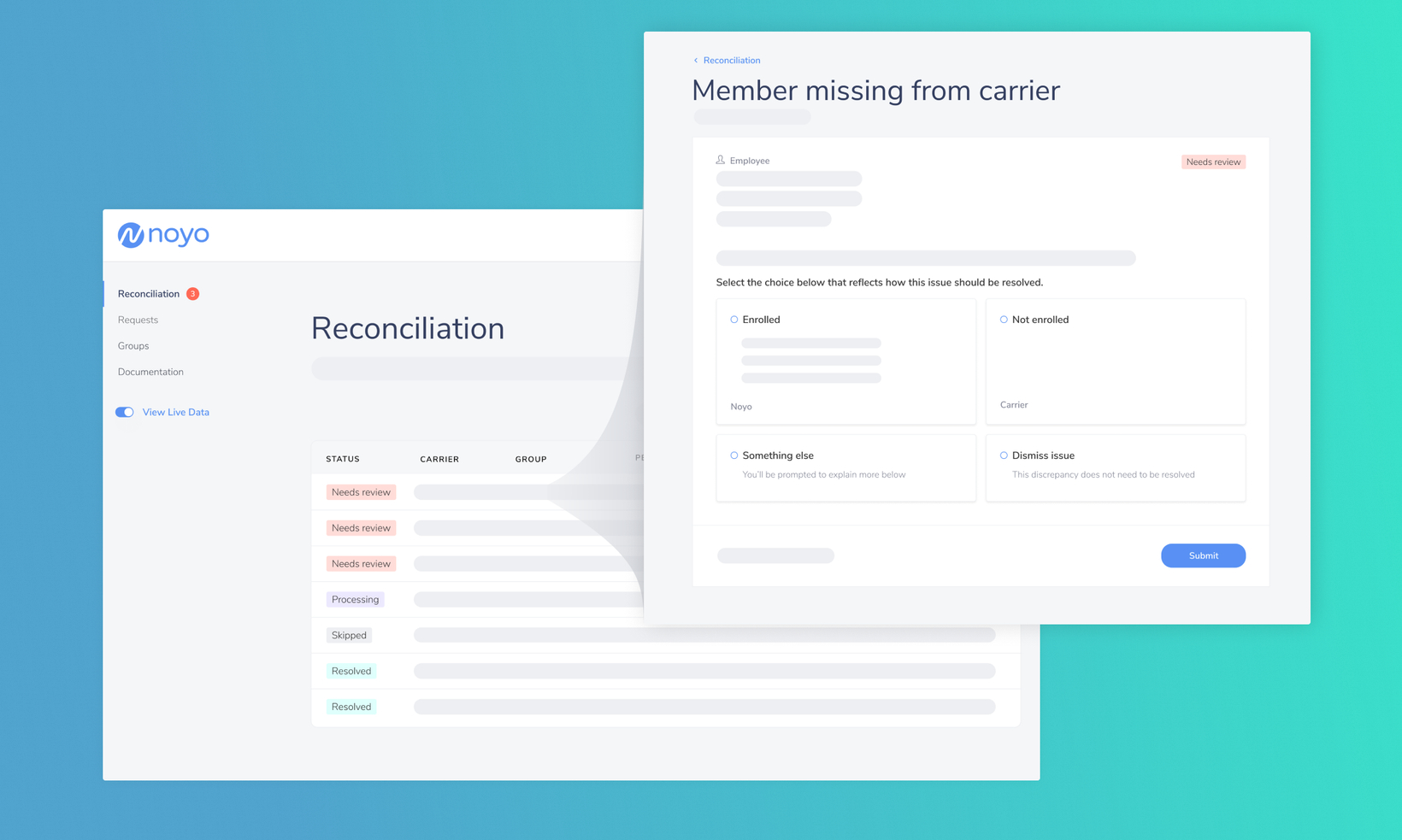
Reconciliation: A powerful new tool for benefits administration platforms
People's lives change rapidly–they move, get married, have children, develop new medical needs–and their insurance coverage needs to keep up. By the time a member discovers an issue with their coverage, they may have already been denied healthcare at a time of need.
Getting the problem resolved can require a cycle of support tickets and claims disputes that are costly for carriers, employers, brokers, and benefits administration platforms.
Noyo already offers round-trip transaction confirmation and proactive audits that monitor for potential data mismatches at the carrier. With Noyo Reconciliation, you can now review and take action on identified issues directly in the Noyo product.
No more emailing and calling back and forth with insurance carriers — you'll be able to resolve most issues with just a few clicks.
Have your customers' backs
Traditional file feed or paper-based methods of data exchange make it difficult to identify and correct problems quickly. In contrast, Noyo's eligibility APIs are specifically designed to provide an unprecedented level of transparency into each change, allowing for automated data validation and a programmatic way to handle mismatches between benefits platforms and carriers.
The key lies with Noyo's ability to both make updates to an insurance carrier's system and read back the state of that system. This closed-loop approach is the first of its kind for our industry and allows us to compare systems in real time.
No more manual investigations
Noyo Reconciliation is available to all Noyo-connected benefits administration platforms. Operations specialists can use Noyo Reconciliation to review issues that Noyo has identified and take action to resolve them in a simple and intuitive interface.
Now, operations personnel can deal with multiple issues per day, stay informed about issues in real time, and track progress through to resolution.
A better customer experience
Insurance carriers who use Noyo to connect to their ben-admin partners will notice fewer disruptions to member coverage, fewer claims disputes, and fewer customer inquiries arising from enrollment problems.
Noyo's APIs are the foundation for a new world of data exchange, and this release is a significant step toward a more connected and transparent future.